Even small employers notsubject to the Affordable Care Act’s (ACA) coverage mandate can’t reimburse employees for nongroup health insurance coverage purchased on a public exchange, the Internal Revenue Service confirmed. But small employers providing premium reimbursement in 2014 are being offered transition relief through mid-2015.
IRS Notice 2015-17, issued on Feb. 18, 2015, is another in a series of guidance from the IRS reminding employers that they will run afoul of the ACA if they use health reimbursement arrangements (HRAs) or other employer payment plans—whether with pretax or post-tax dollars—to reimburse employees for individual policy premiums, including policies available on ACA federal or state public exchanges.
This time the warning is aimed at small employers—those with fewer than 50 full-time employees or equivalent workers. While small organizations are not subject to the ACA’s “shared responsibility” employer mandate to provide coverage or pay a penalty (aka Pay or Play), if they do provide health coverage it must meet a range of ACA coverage requirements.
“The agencies have taken the position that employer payment plans are group health plans, and thus must comply with the ACA’s market reforms,” noted Timothy Jost, J.D., a professor at the Washington and Lee University School of Law, in a Feb. 19 post on the Health Affairs Blog. “A group health plan must under these reforms cover at least preventive care and may not have annual dollar limits. A premium payment-only HRA or other payment arrangement that simply pays employee premiums does not comply with these requirements. An employer that offers such an arrangement, therefore, is subject to a fine of $100 per employee per day. (An HRA integrated into a group health plan that, for example, helps with covering cost-sharing is not a problem).”
Transition Relief
The notice provides transition relief for small employers that used premium payment arrangements for 2014. Small employers also will not be subject to penalties for providing payment arrangements for Jan. 1 through June 30, 2015. These employers must end their premium reimbursement plans by that time. This relief does not extend to stand-alone HRAs or other arrangements used to reimburse employees for medical expenses other than insurance premiums.
No similar relief was given for large employers (those with 50 or more full-time employees or equivalents) for the $100 per day per employee penalties. Large employers are required to self-report their violation on the IRS’s excise tax form 8928 with their quarterly filings.
“Notice 2015-17 recognizes that impermissible premium-reimbursement arrangements have been relatively common, particularly in the small-employer market,” states a benefits brief from law firm Spencer Fane. “And although the ACA created “SHOP Marketplaces” as a place for small employers to purchase affordable [group] health insurance, the notice concedes that the SHOPs have been slow to get off the ground. Hence, this transition relief.”
Subchapter S Corps.
The notice states that Subchapter S closely held corporations may pay for or reimburse individual plan premiums for employee-shareholders who own at least 2 percent of the corporation. “In this situation, the payment is included in income, but the 2-percent shareholder can deduct the premiums for tax purposes,” Jost explained. The 2-percent shareholder may also be eligible for premium tax credits through the marketplace SHOP Marketplace if he or she meets other eligibility requirements.
Tricare
Employers can pay for some or all of the expenses of employees covered by Tricare—a Department of Defense program that provides civilian health benefits for military personnel (including some members of the reserves), military retirees and their dependents—if the payment plan is integrated with a group health plan that meets ACA coverage requirements.
Higher Pay Is Still OK
One option that the IRS will allow employers is to simply increase an employee’s taxable wages in lieu of offering health insurance. “As long as the money is not specifically designated for premiums, this would not be a premium payment plan,” said Jost. “The employer could even give the employee general information about the marketplace and the availability of premium tax credits as long as it does not direct the employee to a specific plan.”
But if the employer pays or reimburses premiums specifically, “even if the payments are made on an after-tax basis, the arrangement is a noncompliant group health plan and the employer that offers it is subject to the $100 per day per employee penalty,” Jost warned.
“Small employers now have just over four months in which to wind down any impermissible premium-reimbursement arrangement,” the Spencer Fane brief notes. “In its place, they may wish to adopt a plan through a SHOP Marketplace. Although individuals may enroll through a Marketplace during only annual or special enrollment periods, there is no such limitation on an employer’s ability to adopt a plan through a SHOP.”
Beginning January 1, 2015, employers have new reporting obligations for health plan coverage, to allow the government to administer the “pay or play” penalties to be assessed against employers that do not offer compliant coverage to their full-time employees.
Even though the penalties only apply if there are 100 or more employees for 2015, employers with 50 or more full-time equivalent employees are required to report for 2015. Also, note this reporting is required even if the employer does not maintain any health plan.
Employers that provide self-funded group health coverage also have reporting obligations, to allow the government to administer the “individual mandate” which results in a tax on individuals who do not maintain health coverage.
These reporting obligations will be difficult for most employers to implement. Penalties for non-compliance are high, so employers need to begin now with developing a plan on how they will track and file the required information.
Pay or Play Reporting. Applicable large employers (ALEs) must report health coverage offered to employees for each month of 2015 in an annual information return due early in 2016. ALEs are employers with 50 or more full-time equivalent (FTE) employees. Employees who average 30 hours are counted as one, and those who average less than 30 hours are combined into an equivalent number of 30 hour employees to determine if there are 50 or more FTE employees. All employees of controlled group, or 80% commonly owned employers, are also combined to determine if the 50 FTE threshold is met.
Individual Mandate Reporting. Self-funded employers, including both ALEs and small employers that are not ALEs, must report each individual covered for each month of the calendar year. For fully-insured coverage, the insurance carrier must report individual month by month coverage. The individual mandate reporting is due early in 2016 for each month of 2015.
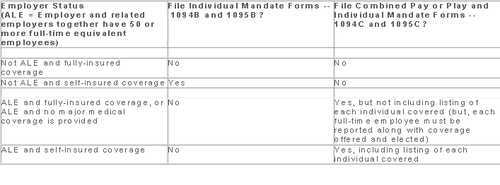
Which Form? ALE employers have one set of forms to report both the pay or play and the individual mandate information – Forms 1094C and 1095C. Insurers and self-insured employers that are not ALEs use Forms 1094B and 1095B to report the individual mandate information. Information about employee and individual coverage provided on these forms must also be reported by the employer to its employees as well as to COBRA and retiree participants. Forms 1095B and 1095C can be used to provide this information, or employers can provide the information in a different format.
The following chart summaries which returns are filed by employers:
Who Reports? While ALE status is determined on a controlled group basis, each ALE must file separate reports. Employers will need to provide insurance carriers, and third party administrators who process claims for self-funded coverage (if they will assist the employer with reporting), accurate data on the employer for whom each covered employee works. If an employee works for more than one ALE in a controlled group, the employer for whom the highest number of hours is worked does the reporting for that employee.
Due Date for Filing. The due date of the forms matches the due dates of Forms W-2, and employers may provide the required employee statements along with the W-2. Employee reporting is due January 31st and reporting to the IRS is due each February 28th, although the date is extended until March 31st if the forms are filed electronically. If the employer files 250 or more returns, the returns must be filed electronically. Reporting to employees can only be made electronically if the employee has specifically consented to receiving these reports electronically.
Penalties. Failure to file penalties can total $200 per individual for whom information must be reported, subject to a maximum of $3 million per year. Penalties will not be assessed for employers who make a good faith effort to file correct returns for 2015.
What Information is Required? For the pay or play reporting, each ALE must file a Form 1094C reporting the number of its full-time employees (averaging 30 hours) and total employees for each calendar month, whether the ALE is in a “aggregated” (controlled) group, a listing of the name and EIN of the top 30 other entities in the controlled group (ranked by number of full-time employees), and any special transition rules being used for pay or play penalties. ALE’s must also file a 1095C for each employee who was a full-time employee during any calendar month of the year. The 1095C includes the employee’s name, address and SSN, and month by month reporting of whether coverage was offered to the employee, spouse and dependents, the lowest premium for employee only coverage, and identification of the safe-harbor used to determine affordability. This information is used to determine pay or play penalty taxes and to verify the individuals’ eligibility for subsidies toward coverage costs on the Federal and state exchanges.
If the ALE provides self-funded coverage, the ALE must also report on the 1095C the name and SSN of each individual provided coverage for each calendar month. If an employer is not an ALE, but is self-funded, the name and SSN of each covered individual is reported on the 1095B and the 1094B is used to transmit the forms 1095B to the IRS.
A chart is available that sets out what data must be reported on each form, to help employers determine what information they need to track. Click here to access the chart.
Next Steps. Employers will need to determine how much help their insurance carrier or TPA can provide with the reporting, and then the employer’s HR, payroll and IT functions will need to work together to be sure the necessary information is being tracked and can be produced for reporting in January 2016.
The Affordable Care Act will require Applicable Large Employers (i.e. large employers subject to the employer mandate) and employers sponsoring self-insured plans to comply with new annual IRS reporting requirements. The first reporting deadline will be February 28, 2016 as to the data employers collect during the 2015 calendar year. The reporting provides the IRS with information it needs to enforce the Individual Mandate (i.e. individuals are penalized for not having health coverage) and the Employer Mandate (i.e. large employers are penalized for not offering health coverage to full-time employees). The IRS will also require employers who offer self-insured plans to report on covered individuals.
Large employers and coverage providers must also provide a written statement to each employee or responsible individual (i.e. one who enrolls one or more individuals) identifying the reported information. The written statement can be a copy of the Form.
The IRS recently released draft Forms 1094-C and 1095-C and draft Forms 1094-B and 1095-B, along with draft instructions for each form.
Which Forms Do I File?
When?
Statements to employees and responsible individuals are due annually by January 31. The first statements are due January 31, 2016.
Forms 1094-B, 1095-B, 1094-C and 1095-C are due annually by February 28 (or by March 31, if filing electronically). The first filing is due by February 28, 2016 (or March 31, 2016, if filing electronically).
Even though the forms are not due until 2016, the annual reporting will be based on data from the prior year. Employers need to plan ahead now to collect data for 2015. Many employers have adopted the Look Back Measurement Method Safe Harbor (“Safe Harbor”) to identify full-time employees under the ACA. The Safe Harbor allows employers to “look back” on the hours of service of its employees during 2014 or another measurement period. There are specific legal restrictions regarding the timing and length of the periods under the Safe Harbor, so employers cannot just pick random dates. Employers also must follow various rules to calculate hours of service under the Safe Harbor. The hours of service during the measurement period (which is likely to include most of 2014) will determine whether a particular employee is full-time under the ACA during the 2015 stability period. The stability period is the time during which the status of the employee, as full-time or non-full-time, is locked in. In 2016, employers must report their employees’ full-time status during the calendar year of 2015. Therefore, even though the IRS forms are not due until 2016, an employee’s hours of service in 2014 will determine how an employer reports that employee during each month of 2015. Employers who have not adopted the Safe Harbor should consider doing so because it allows an employer to average hours of service over a 12-month period to determine the full-time status of an employee. If an employer does not adopt the Safe Harbor, the IRS will require the employer to make a monthly determination, which is likely to increase an employer’s potential exposure to penalties.
What Must the Employer Report?
Form 1095-C
There are three parts to Form 1095-C. An applicable large employer must file one Form 1095-C for each full-time employee. If the applicable large employer sponsors self-insured health plans, it must also file Form 1095-C for any employee who enrolls in coverage regardless of the full-time status of that employee.
Form 1095-C requires the employer to identify the type of health coverage offered to a full-time employee for each calendar month, including whether that coverage offered minimum value and was affordable for that employee. Employers must use a code to identify the type of health coverage offered and applicable transition relief.
Employers that offer self-insured health plans also must report information about each individual enrolled in the self-insured health plan, including any full-time employee, non-full-time employee, employee family members, and others.
Form 1094-C
Applicable large employers use Form 1094-C as a transmittal to report employer summary information and transmit its Forms 1095-C to the IRS. Form 1094-C requires employers to enter the name and contact information of the employer and the total number of Forms 1095-C it submits. It also requires information about whether the employer offered minimum essential coverage under an eligible employer-sponsored plan to at least 95% of its full-time employees and their dependents for the entire calendar year, the number of full-time employees for each month, and the total number of employees (full-time or non-full-time) for each month.
Form 1095-B
Employers offering self-insured coverage use Form 1095-B to report information to the IRS about individuals who are covered by minimum essential coverage and therefore are not liable for the individual shared responsibility payment. These employers must file a Form 1095-B for eachindividual who was covered for any part of the calendar year. The employer must make reasonable efforts to collect social security numbers for covered individuals.
Form 1094-B
Employers who file Form 1095-B will use Form 1094-B as a transmittal form. It asks for the name of the employer, the employer’s EIN, and the name, telephone number, and address of the employer’s contact person.
Failure to Report – What Happens?
The IRS will impose penalties for failure to timely provide correct written statements to employees. The IRS will also impose penalties for failure to timely file a correct return. For the 2016 reporting on 2015 data, the IRS will not impose a penalty for good faith compliance. However, the IRS specified that good faith compliance requires that employers provide the statements and file the returns.
On November 4, 2014, the IRS released Notice 2014-69 which outlines that health plans that fail to provide substantial coverage for in-patient hospitalization services or for physician services (or both) referred to as Non-Hospital/Non-Physician Services Plan) are now not considered as providing the minimum value coverage as intended by the minimum value plan requirements for the employer mandate under ACA.
For employers who have already entered into a binding written commitment to adopt, or have begun enrolling employees in, a Non-Hospital/Non-Physician Services Plan prior to November 4, 2014, they will not be penalized for not meeting the employer mandate for the 2015 plan year if that plan year begins no later than March 1, 2015. This is based on the employer’s reliance on the results of the Minimum Value Calculator (a Pre-November 4, 2014 Non-Hospital/Non-Physician Services Plan) as outlined in previous guidance.
For employers who have not entered in to a written commitment to adopt, have not begun enrolling employees in a Non-Hospital/Non-Physician Services Plan on or after November 4, 2014, or have a plan year that begins after March 1,2015, no relief will be given under the employer mandate.
Pending final regulations, employees will not be required to treat a Non-Hospital/Non-Physician Services Plan as providing minimum value coverage for purposes of determining their eligibility for a premium tax credit “aka premium subsidy” in the Marketplace.
An employer that offers a Non-Hospital/Non-Physician Services Plan (including a Pre-November 4, 2014 Non-Hospital/Non-Physician Services Plan) to an employee:
(1) must not state or imply in any disclosure that the offer of coverage under the Non-Hospital/Non-Physician Services Plan prevents an employee from obtaining a premium tax credit, if otherwise eligible, and
(2) must timely correct any prior disclosures that stated or implied that the offer of the Non-Hospital/Non-Physician Services Plan would prevent an otherwise tax-credit-eligible employee from obtaining a premium tax credit.
Without such a corrective disclosure, a statement a Non-Hospital/Non-Physician Services Plan provides minimum value will be considered to imply that the offer of such a plan prevents employees from obtaining a premium tax credit/subsidy. However, an employer that also offers an employee another plan that is not a Non-Hospital/Non/-Physician Services Plan and that is affordable and provides minimum value is permitted to advise the employee that the offer of this other plan will or may preclude the employee from obtaining a premium tax credit.
With Congress in its summer recess, now is a good time to reflect on the top ACA issues worth monitoring as 2015 quickly approaches. Here are a handful of key issues to watch:
Dueling Court Cases on Federal Subsidies
One issue grabbing national headlines is the dueling decisions coming out of the U.S. Court of Appeals for the District of Columbia (Halbig v. Burwell) and the U.S. Court of Appeals for the Fourth Circuit (King v. Burwell) on missing language in the ACA that would have authorized the federal government to provide premium subsidies to individuals who sign up for health plans through the federal Exchanges. The legal issue in these court cases is whether the ACA premium tax credit (aka subsidy) is available to those individuals who enroll in qualified health plans (QHP) through state operated Exchanges or if it is available only to those to enroll in a QHP through a federally funded Exchange.
A primary concern is that a significant number of people in about two-thirds of the states (who did not set up a state-run Exchange) rely on the subsidy to purchase a plan in the federal Exchange. Specifically, the ACA’s employer mandate penalty of $3000 is based upon an employer having an employee seek coverage through an Exchange and receive the federal premium subsidy. In general, the employer mandate requires that “applicable large employers” offer their full-time employees minimum essential coverage or potentially pay a tax penalty. However, according to the statutory text of the ACA, the penalties under the employer mandate are triggered only if an employee receives a subsidy to purchase coverage through an Exchange established by the states. Both cases are being appealed to higher courts and will likely be consolidated into one case to be heard by the U.S. Supreme Court in the not so distant future.
In an interesting development, a video surfaced last week featuring one of the ACA’s chief architects (John Gruber) saying that health insurance subsidies should only be available in those states who opt to build and implement state-based Exchanges to gain participation. The idea was to create an incentive to have states actively involved in the hosting of an Exchange, rather than relying on the federal government to operate the Exchanges in each state. Whether this video will be used as evidence to uphold the argument that subsidies can only be offered by state-based Exchanges remains to be seen.
Lack of Back End Software for Federal Exchange
Of course, one of the big news stories in 2013 and early 2014 was the substandard launch of the federal Exchange, which led to many Americans having to wait to be enrolled in an ACA-compliant health plan. Although some technical snafus have been addressed, there are many that still remain. For example, a top White House official recently told Congress that the automated system that is supposed to send premium payments to insurance companies is still under development, and they did not have a completion date for it yet. The lack of an electronic verification process is only one part of the “backend” software that is still problematic five years after PPACA was passed.
Future of Navigators in Comparison with the Value of Brokers
Several recent studies have touted the benefits of using third parties, such as Brokers, to help consumers find coverage under the ACA. Some of these studies have focused on the usefulness of using Brokers/Agents over the benefits of using Navigators. A recent Urban Institute study found that health insurance Brokers were the most helpful in providing health insurance Exchange information when compared to other types of resources, including Navigators and website content. However, there are other published studies showcasing how Navigators have been useful to consumers. That being said, Brokers have assumed an integral role supporting millions of Americans in securing and maintaining coverage for many decades, and continue to be knowledgeable resources, as they are licensed in the states they operate in, whereas Navigators are not required to meet the same licensing standards as Brokers/Agents. It will be interesting to see what the future holds for Navigators, who are not as experienced and who are, in the end, dependent upon federal grants to provide their services.
Provider Access Issues & Emergency Room Over-Usage
A number of public policymakers have raised concerns recently about the fact that there are shortages of key physicians and other providers and as a result is causing a increase in non-emergent patient visits to expensive ER departments. A recent story in the New York Times highlighted similar concerns, saying the ACA cannot change the fact that visiting an emergency room may be easier than seeing a primary care physician in some instances or locations. Other stories and studies highlight how the ACA and health care reform initiatives can affect access to providers in many different ways, such as changing reimbursement levels, improving the availability of certain types of specialists, or re-educating the patient to move from visiting the ER department to either making an appointment ahead-of-time or visiting a less expensive Urgent Care center for care.
Premium Rate Increases
Another critical issue to monitor are premium increases that might be occurring in spite of the initial promises that the ACA would lower health care costs. Health plans have begun publishing proposed rates for 2015, resulting in a recent flurry of news articles and reports addressing the impact of the ACA on insurance premiums.
The Wall Street Journal published a front page report discussing the ACA’s impact on premium increases earlier this summer, saying, “Hundreds of thousands of consumers nationwide, who bought insurance plans under the Affordable Care Act, will face a choice this fall: swallow higher premiums to stay in their plans or save money by switching.”
The Journal goes on to say that a new picture is emerging in 10 states where 2015 premium insurance rates for individual plans have been filed, “In all but one (state), the largest health insurer is proposing to increase premiums between 8.5% to 22.8% next year.” Ironically, smaller health plans are reducing their 2015 rates in the same market in an attempt to gain market share.
The significance of this trend is underscored in a statement released earlier this summer by Karen Ignagni, president & CEO of America’s Health Insurance Plans (AHIP), in which she expressed concerns about keeping health insurance affordable for patients. “Affordability remains a top priority for consumers when it comes to their health care,” she said.
Bonus: Be Sure To Watch The Political Races
With the ACA’s continued challenges, the ups and downs of the U.S. economy, key world events in the Middle East, and other confounding variables, one has to wonder what will happen during the mid-year elections this fall. As reported by CNN and other news outlets, the ACA became an key issue in Obama’s 2012 re-election victory as well as Democrats picking up seats in the Senate and House in that election.
As November 3, 2015 approaches, many different messages could be sent back to the White House and Congress. If Republicans take over the Senate and retain control of the House, how will this impact the ACA over the next several years? If the congressional houses remain split, we may have less going on by either political party. How will the state-level elections impact the ACA and state-run Exchanges? Only time will tell.
Under the Patient Protection and Affordable Care Act (PPACA), beginning in 2015, certain large employers who do not offer affordable health insurance that provides minimum value to their full-time employees may be subject to significant penalties.
In a nutshell, in 2015, “applicable large employers” will be subject to an annualized employer “shared responsibility” penalty of $2,000 (indexed) per full-time employee (minus the first 80 full-time employees in 2015) if the employer does not offer health insurance to at least 70% of their full-time employees and their dependents. This amount will be increase from 70% to 95% after 2015. This is commonly referred to as the “Pay or Play” penalty.
Even if an applicable large employer offers insurance coverage to full-time employees, the employer still could be subject to an annualized penalty of $3,000 (indexed) per employee who receives an Exchange subsidy if the offered employer-sponsored health coverage does not meet minimum value standards or is not affordable. This $3000 penalty is capped at the amount that would apply if the $2,000 penalty described above were to apply.
What should an employer do now to prepare for these penalties?
(A) Determine if they are an “applicable large employer” -To do this, employers should count both full-time employees and part-time employee hours as follows:
1) Count the full-time employees for each month in the prior year.
2) Count the full-time equivalents for each month in the prior year.
a) Add total hours for non-full-time employees but count no more than 120 hours per month for any one non-full-time employee.
b) Divide the number obtained in (a) by 120. This is the full-time equivalent number.
3) Add the numbers obtained in (1) and (2) above (i.e., the full-time employee and full-time equivalent numbers) for each month.
4) Add the 12 sums obtained in (3) and divide by 12. This is the average number of full-time employees and full-time equivalents.
5) If this number obtained in (4) is under 50 (or under 100 for the 2015 determination for certain employers), the employer is not an applicable large employer for the year being determined.
Note: The applicable large employer is determined on a controlled group basis. For example, if there are three companies, each of which is wholly owned by the same parent company, the companies are all considered one employer for this calculation. Also note that, special transition rules apply in determining applicable large employer status for 2015 and that a special seasonal employee exception may apply even if the threshold in (5) is exceeded.
(B) If an employer will be an applicable large employer in 2015, it should determine whether it could be subject to penalties in 2015. For example, the employer should review its group health plan to determine if the insurance coverage is “offered” to full-time employees meets minimum value standards and is considered affordable to employees.
© An employer also will need to address how it will determine the full-time status of employees – will it use the “monthly measurement period” or the “look back measurement period.” This is particularly important for employers who have many variable-hour employees or seasonal employees.
(D) If the employer’s group health plan does not meet the threshold tests to avoid the penalties noted above, the employer should evaluate whether it wants to restructure its health care offerings or pay the penalties (which are non-deductible).
(E) Finally, employers should review their data collection procedures to ensure that they will be able to report the healthcare information required to be reported for 2015 (the actual reporting will occur in 2016 for the 2015 calendar year). Insurers, sponsors of self-insured plans, and other entities that provide minimum essential coverage during a calendar year will be required to report certain information to the IRS and to participants. In addition, applicable large employers will be required to report about the coverage they provide to both the IRS and to their employees. Drafts of the IRS forms to be used in reporting this information have recently been published (Form 1095-B, Form 1095-B Transmittal, Form 1095-C, Form 1095-C Transmittal). Employers should review these forms to understand the data that will need to be reported.
It is not too late for employers to take action now to avoid penalties in 2015.
The Affordable Care Act (ACA) imposes significant information reporting responsibilities on employers starting with the 2015 calendar year. One reporting requirement applies to all employer-sponsored health plans, regardless of the size of the employer. A second reporting requirement applies only to large employers, even if the employer does not provide health coverage. The IRS is currently developing new systems for reporting the required information and recently released draft forms, however instructions have yet to be released.
Information returns
The new information reporting systems will be similar to the current Form W-2 reporting systems in that an information return (Form 1095-B or 1095-C) will be prepared for each applicable employee, and these returns will be filed with the IRS using a single transmittal form (Form 1094-B or 1094-C). Electronic filing is required if the employer files at least 250 returns. Employers must file these returns annually by Feb. 28 (March 31 if filed electronically). Therefore, employers will be filing these forms for the 2015 calendar year by Feb. 28 or March 31, 2016 respectively. A copy of the Form 1095, or a substitute statement, must be given to the employee by Jan. 31 and can be provided electronically with the employee’s consent. Employers will be subject to penalties of up to $200 per return for failing to timely file the returns or furnish statements to employees.
The IRS released drafts of the Form 1095-B and Form 1095-C information returns, as well as the Form 1094-B and Form 1094-C transmittal returns, in July 2014 and is expected to provide instructions for the forms in August 2014. According to the IRS, both the forms and the instructions will be finalized later this year.
Health coverage reporting requirement
The health coverage reporting requirement is designed to identify employees and their family members who are enrolled in minimum essential health coverage. Employees who are offered coverage, but decline the coverage, are not reported. The IRS will use this information to determine whether the employees are exempt from the individual mandate penalty due to having health coverage for themselves and their family members.
Insurance companies will prepare Form 1095-B (Health Coverage) and Form 1094-B (Transmittal of Health Coverage Information Returns) for individuals covered by fully-insured employer-sponsored group health plans. Small employers with self-insured health plans will use Form 1095-B and Form 1094-B to report the name, address, and Social Security number (or date of birth) of employees and their family members who have coverage under the self-insured health plan. However, large employers (as defined below) with self-insured health plans will file Forms 1095-C and 1094-C in lieu of Forms 1095-B and 1094-B.
Large employer reporting requirement
“Applicable large employer members (ALE)” are subject to the reporting requirement if they offer an insured or self-insured health plan, or do not offer any group health plan. ALE members are those employers that are either an applicable large employer on their own or are members of a controlled or affiliated service group with an ALE (regardless of the number of employees of the group member). ALEs are those that had, on average, at least 50 full-time employees (including full-time equivalent “FTE” employees) during the preceding calendar year. Full-time employees are those who work, on average, at least 30 hours per week. Employers with fewer than 50 full-time employees and equivalents are not applicable large employers and, thus, are exempt from this health coverage reporting requirement.
As referenced above, an employer’s status as an ALE is determined on a controlled or affiliated service group basis. For example, if Company A and Company B are members of the same controlled group and Company A has 100 employees and Company B has 20 employees, then A and B are both members of an ALE. Consequently, Company A and Company B must each file the information returns.
Each ALE member must file Form 1095-C (Employer-Provided Health Insurance Offer and Coverage) and Form 1094-C (Transmittal of Employer-Provided Health Insurance Offer and Coverage Information Returns) with the IRS for each calendar year. The IRS will use this information to determine whether (1) the employer is subject to the employer mandate penalty, and (2) an employee is eligible for a premium tax credit on insurance purchased through the new health insurance exchange. ALEs with fewer than 100 full-time employees are generally eligible for transition relief from the employer mandate penalty for their 2015 plan year. Nonetheless, these employers are still required to file Forms 1095-C and 1094-C for the 2015 calendar year.
The employer mandate penalty can be imposed on any ALE member that does not offer affordable, minimum value health coverage to all of its full-time employees starting in 2015. Health coverage is affordable if the amount that the employer charges an employee for self-only coverage does not exceed 9.5 percent of the employee’s Form W-2 wages, rate of pay, or the federal poverty level for the year. A health plan provides minimum value if the plan is designed to pay at least 60 percent of the total cost of medical services for a standard population. In the case of a controlled or affiliated service group, the employer mandate penalties apply to each member of the group individually.
ALE members must prepare a Form 1095-C for each employee. The return will report the following information:
An ALE member will file with the IRS one Form 1094-C transmitting all of its Forms 1095-C. The Form 1094-C will report the following information:
As noted above, each ALE member is required to file Forms 1095-C and 1094-C for its own employees, even if it participates in a health plan with other employers (e.g., when the parent company sponsors a plan in which all subsidies participate). Special rules apply to multiemployer plans for collectively-bargained employees.
Action required
In light of the complexity of the new information reporting requirements, it is recommended that employers should begin taking steps now to prepare for the new reporting requirements:
Starting in 2015, the Affordable Care Act (ACA) requires applicable large employers to offer affordable, minimum value health coverage to their full time employees (and dependents) or pay a penalty. The employer penalty rules are also known as the employer mandate or the “pay or play” rules.
Effective in 2014, affordability of health coverage is used to determine whether an individual is:
On July 24, 2014, the IRS released Revenue Procedure 2014-37 to index the ACA’s affordability percentages for 2015.
For plan years beginning in 2015, an applicable large employer’s health coverage will be considered affordable under the pay or play rules if the employee’s requires contribution to the plan does not exceed 9.56 percent of the employee’s household income for the year. The current affordability percentage for 2014 is 9.5 percent.
Applicable large employers can use one of the IRS’ affordability safe harbors to determine whether their health plans will satisfy the 9.56 percent requirement for 2015 plan years, if requirements for the applicable safe harbor are met.
This adjusted affordability percentage will also be used to determine whether an individual is eligible for a premium tax credit for 2015. Individuals who are eligible for employer-sponsored coverage that is affordable and provides minimum value are not eligible for a premium tax credit in the Exchange.
Also, Revenue Procedure 2014-37 adjusts the affordability percentage for the exemption from the individual mandate for individuals who lack access to affordable minimum essential coverage. For plan years beginning in 2015, coverage is unaffordable for purposes of the individual mandate if it exceeds 8.05 percent of household income.
Employer Mandate
The pay or play rules apply only to applicable large employers. An “applicable large employer” is an employer with, on average, at least 50 full-time employees (including full-time equivalents) during the preceding calendar year. Many applicable large employers will be subject to the pay or play rules starting in 2015. However, applicable large employers with fewer than 100 full-time employees may qualify for an additional year, until 2016, to comply with the employer mandate.
Affordability Determination
The affordability of health coverage is a key point in determining whether an applicable large employers will be subject to a penalty.
For 2014, the ACA provides that an employer’s health coverage is considered affordable if the employee’s required contribution to the plan does not exceed 9.5 percent of the employee’s household income for the taxable year. The ACA provides that, for plan year beginning after 2014, the IRS must adjust the affordability percentage to reflect the excess of the rate of premium growth over the rate of income growth for the preceding calendar year.
As noted above, the IRS has adjusted the affordability percentage for plan years beginning in 2015 to 9.56 percent. The affordability text applies only to the portion of the annual premiums for self-only coverage and does not include any additional cost for family coverage. Also, if an employer offers multiple health coverage options, the affordability test applies to the lowest-cost option that also satisfies the minimum value requirement.
Affordability Safe Harbors
Because an employer generally will not know an employee’s household income, the IRS created three affordability safe harbors that employers may use to determine affordability based on information that is available to them.
The affordability safe harbors are all optional. An employer may choose to use one or more of the affordability safe harbors for all its employees or for any reasonable category of employees, provided it does so on a uniform and consistent basis for all employees in a category.
The affordability safe harbors are:
Individual Mandate
Beginning in 2014, the ACA requires most individuals to obtain acceptable health insurance coverage for themselves and their family members or pay a penalty. This rule is often referred to as the “individual mandate”. Individual may be eligible for an exemption from the penalty in certain circumstances.
Under the ACA, individuals who lack access to affordable minimum essential coverage are exempt from the individual mandate. For purposes of this exemption, coverage is considered affordable for an employee in 2014 if the required contribution for the lowest-cost, self-only coverage does not exceed 8 percent of household income. For family members, coverage is considered affordable in 2014 if the required contribution for the lowest-cost family coverage does not exceed 8 percent of household income. This percentage will be adjusted annually after 2014.
For plan years beginning in 2015, the IRS has increased this percentage from 8 percent to 8.05 percent.
Many employers originally thought they could shift health costs to the government by sending their employees to a health insurance Exchange/Marketplace with a tax-free contribution of cash to help pay premiums, but the Obama administration has squashed this idea in a new ruling. Such arrangements do not satisfy requirements under the Affordable Care Act (ACA), the Obama administration said, and employers could now be subject to a tax penalty of $100 a day — or $36,500 a year — for each employee who goes into the individual Marketplace/Exchange for health coverage.
The ruling this month, by the Internal Revenue Service, prevents any “dumping” of employees into the exchanges by employers.
Under a main provision in the health care law, employers with 50 or more employees are required to offer health coverage to full-time workers, or else the employer may be subject to penalties.
Many employers had concluded that it would be cheaper to provide each employee with a lump sum of money to buy insurance on an exchange, instead of providing employer-sponsored health coverage directly to employees as they had in the past.
But the Obama administration has now raised objections in an authoritative Q&A document recently released by the IRS, in consultation with other agencies.
The health law, known as the Affordable Care Act (ACA), was intended to build on the current system of employer-based health insurance. The administration wants employers to continue to provide coverage to workers and their families and do not see the introduction of ACA as an eventual erosion of employer provided coverage.
Employer contributions to sponsored health coverage, which averages more than $5,000 a year per employee, are not counted as taxable income to workers. But the IRS has said employers could not meet their obligations under ACA by simply reimbursing employees for some or all of their premium costs from the marketplace/exchange.
Christopher E. Condeluci, a former tax and benefits counsel to the Senate Finance Committee, said the recent IRS ruling was significant because it made clear that “an employee cannot use tax-free contributions from an employer to purchase an insurance policy sold in the individual health insurance market, inside or outside an exchange.”
If an employer wants to help employees buy insurance on their own, Condeluci said, they can give the employee higher pay, in the form of taxable wages. But in such cases, he said, the employer and the employee would owe payroll taxes on those wages, and the change could be viewed by workers as reducing a valuable benefit.
A tax partner from a large accounting firm has also said the ruling could disrupt reimbursement arrangements used in many industries.
For decades, many employers have been assisting employees by reimbursing them for health insurance premiums and out-of-pocket costs associated with their health coverage. The new federal ruling eliminates many of those arrangements, commonly known as Health Reimbursement Arrangements (HRAs) or employer payment plans, by imposing an unusually punitive penalty. The IRS has said that these employer payment plans are considered to be group health plans, but they do not satisfy requirements of the Affordable Care Act for health coverage.
Under the law, insurers may not impose annual limits on the dollar amount of benefits for any individual, and they must provide certain preventive services, like mammograms and colon cancer screenings, without co-payments or other charges.
But the administration has said that employer payment plans or HRAs do not meet these requirements.
This ruling was released as the Obama administration rushed to provide guidance to employers and insurers who are beginning to review coverage options for 2015.
The Department of Health and Human Services said it would provide financial assistance to certain insurers that experience unexpected financial losses this year. Administration officials hope the payments will stabilize medical premiums and prevent rate increases that are associated with the required policy changes as a result of ACA.
Republicans want to block these payments, however, as they see them as a bailout for insurance companies who originally supported the president’s health care law.
Stay tuned for more updates on ACA as they are released. Should you have any questions, please do not hesitate to contact our office.
Keeping up with changes under the Affordable Care Act (ACA) is a challenge for all employers. Here are the top five issues you should specifically pay attention to as healthcare reform rolls out.
The Employer Mandate
Under the ACA, large employers will be required to provide affordable healthcare insurance that meets minimum value to all full-time employees beginning in 2015. Final regulations issued in February clarify most aspects of how the mandate will be implemented.
The Individual Mandate
Beginning January 1, 2014, all individuals are required to carry qualified health insurance known as “minimum essential coverage” or face penalties when they file taxes in the spring of 2015. In 2014, the penalty for noncompliance will be the greater of $95 per uninsured person or 1% of household income over the filing threshold. This penalty will rise in 2015 and again in 2016.
Wellness Programs
As health insurance costs rise, wellness programs are gaining popularity, however be cautious when designing and maintaining a wellness program because they must conform to new ACA requirements and existing HIPAA nondiscrimination requirements.
Reporting Requirements
Beginning in the spring of 2016, large employers will face a new reporting requirement for the 2015 calendar year. The Form 6056 will ask for information including:
Automatic Enrollment And Nondiscrimination Regulations
Though enforcement of the automatic enrollment and nondiscrimination provisions of the ACA has not started, keep an eye out for regulations that will trigger compliance obligations. Employers with over 100 employees should anticipate that in the next few years, they will be required to automatically enroll all full-time employees for health insurance coverage.
In addition, employers who offer varying levels of coverage or employer-provided subsidies based on classes of employees need to watch for nondiscrimination regulations.
Please contact our office if you have any questions on how Healthcare Reform will affect you or your business.