Page 1 of 1
Transparency in Coverage mandates and COVID-19 considerations continue to dominate the discussion in the employee benefits compliance space this summer, but an “old faithful” reporting requirement looms soon: the Patient-Centered Outcomes Research Institute (PCORI) filing and fee. The Affordable Care Act imposes this annual per-enrollee fee on insurers and sponsors of self-funded medical plans to fund research into the comparative effectiveness of various medical treatment options.
The typical due date for the PCORI fee is July 31, but because that date falls on a Sunday in 2022, the effective due date is pushed to the next business day, which is Aug. 1.
The filing and payment due by Aug. 1, 2022, is required for policy and plan years that ended during the 2021 calendar year. For plan years that ended Jan. 1, 2021 – Sept. 30, 2021, the fee is $2.66 per covered life. For plan years that ended Oct. 1, 2021 – Dec. 31, 2021 (including calendar year plans that ended Dec. 31, 2021), the fee is calculated at $2.79 per covered life.
Insurers report on and pay the fee for fully insured group medical plans. For self-funded plans, the employer or plan sponsor submits the fee and accompanying paperwork to the IRS. Third-party reporting and payment of the fee (for example, by the self-insured plan sponsor’s third-party claim payor) is not permitted.
An employer that sponsors a self-insured health reimbursement arrangement (HRA) along with a fully insured medical plan must pay PCORI fees based on the number of employees (dependents are not included in this count) participating in the HRA, while the insurer pays the PCORI fee on the individuals (including dependents) covered under the insured plan. Where an employer maintains an HRA along with a self-funded medical plan and both have the same plan year, the employer pays a single PCORI fee based on the number of covered lives in the self-funded medical plan and the HRA is disregarded.
The IRS collects the fee from the insurer or, in the case of self-funded plans, the plan sponsor in the same way many other excise taxes are collected. Although the PCORI fee is paid annually, it is reported (and paid) with the Form 720 filing for the second calendar quarter (the quarter ending June 30). Again, the filing and payment is typically due by July 31 of the year following the last day of the plan year to which the payment relates, but this year the due date pushes to Aug. 1.
IRS regulations provide three options for determining the average number of covered lives: actual count, snapshot and Form 5500 method.
Actual count: The average daily number of covered lives during the plan year. The plan sponsor takes the sum of covered lives on each day of the plan year and divides the number by the days in the plan year.
Snapshot: The sum of the number of covered lives on a single day (or multiple days, at the plan sponsor’s election) within each quarter of the plan year, divided by the number of snapshot days for the year. Here, the sponsor may calculate the actual number of covered lives, or it may take the sum of (i) individuals with self-only coverage, and (ii) the number of enrollees with coverage other than self-only (employee-plus one, employee-plus family, etc.), and multiply by 2.35. Further, final rules allow the dates used in the second, third and fourth calendar quarters to fall within three days of the date used for the first quarter (in order to account for weekends and holidays). The 30th and 31st days of the month are both treated as the last day of the month when determining the corresponding snapshot day in a month that has fewer than 31 days.
Form 5500: If the plan offers family coverage, the sponsor simply reports and pays the fee on the sum of the participants as of the first and last days of the year (recall that dependents are not reflected in the participant count on the Form 5500). There is no averaging. In short, the sponsor is multiplying its participant count by two, to roughly account for covered dependents.
The U.S. Department of Labor says the PCORI fee cannot be paid from ERISA plan assets, except in the case of union-affiliated multiemployer plans. In other words, the PCORI fee must be paid by the plan sponsor; it cannot be paid in whole or part by participant contributions or from a trust holding ERISA plan assets. The PCORI expense should not be included in the plan’s cost when computing the plan’s COBRA premium. The IRS has indicated the fee is, however, a tax-deductible business expense for sponsors of self-funded plans.
Although the DOL’s position relates to ERISA plans, please note the PCORI fee applies to non-ERISA plans as well and to plans to which the ACA’s market reform rules don’t apply, like retiree-only plans.
The filing and remittance process to the IRS is straightforward and unchanged from last year. On Page 2 of Form 720, under Part II, the employer designates the average number of covered lives under its “applicable self-insured plan.” As described above, the number of covered lives is multiplied by the applicable per-covered-life rate (depending on when in 2021 the plan year ended) to determine the total fee owed to the IRS.
The Payment Voucher (720-V) should indicate the tax period for the fee is “2nd Quarter.”
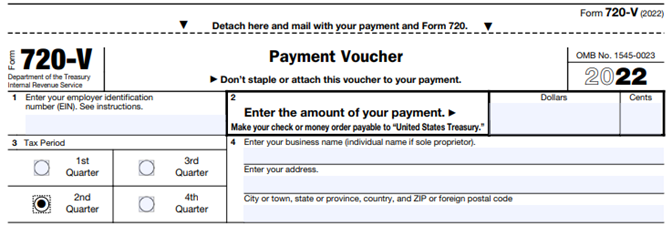
Failure to properly designate “2nd Quarter” on the voucher will result in the IRS’ software generating a tardy filing notice, with all the incumbent aggravation on the employer to correct the matter with IRS.
An employer that overlooks reporting and payment of the PCORI fee by its due date should immediately, upon realizing the oversight, file Form 720 and pay the fee (or file a corrected Form 720 to report and pay the fee, if the employer timely filed the form for other reasons but neglected to report and pay the PCORI fee). Remember to use the Form 720 for the appropriate tax year to ensure that the appropriate fee per covered life is noted.
The IRS might levy interest and penalties for a late filing and payment, but it has the authority to waive penalties for good cause. The IRS’s penalties for failure to file or pay are described here.
The IRS has specifically audited employers for PCORI fee payment and filing obligations. Be sure, if you are filing with respect to a self-funded program, to retain documentation establishing how you determined the amount payable and how you calculated the participant count for the applicable plan year.
The health reform law imposes a number of fees, taxes and other assessments on health insurance companies and sponsors of self-funded health plans to help subsidize a number of endeavors. One such fee funds the Patient-Centered Outcomes Research Institute (PCORI).
The PCORI fee is $2.17 per covered life for plan years ending on or after Oct. 1, 2015, and must be reported on (and remitted with) IRS Form 720 by Aug. 1, 2016 (the deadline is July 31, but since July 31 falls on a weekend, the form is due by the next business day, Aug. 1). For self-funded plans, the employer/plan sponsor will be responsible for submitting the fee and accompanying paperwork to the IRS. Third-party reporting and payment of the fee is not permitted for self-funded plans.
The process for remitting payment by sponsors of self-funded plans is described in more detail below.
The IRS will collect the fee from the insurer or, in the case of self-funded plans, the plan sponsor in the same way many other excise taxes are collected. The fees are reported and paid annually on IRS Form 720 by July 31 of the year following the last day of the plan year. This year the fee is due by Aug. 1.
The fee due on Aug. 1, 2016 is $2.17 per covered life for plan years ending before Oct. 1, 2016, and on or after Oct. 1, 2015. For plan years ending before Oct. 1, 2015, the fee due on Aug. 1, 2016, is $2.08 per covered life under the plan. IRS regulations provide three options for determining the average number of covered lives (actual count, snapshot and Form 5500 method).
The Form 720 must be filed by July 31 (Aug. 1 in 2016) of the calendar year immediately following the last day of the plan year. For example, calendar year plans will owe a fee of $2.17 per covered life by Aug. 1, 2016. Plans that operate on years that begin the first day of any month from February through October will be paying a $2.08 per covered life fee with the Aug. 1, 2016, filing.
The U.S. Department of Labor believes the fee cannot be paid from plan assets. In other words, the PCORI fee must be paid by the plan sponsor; it is not a permissible expense of a self-funded plan and cannot be paid in whole or part by participant contributions. The PCORI expense should not be included in the plan’s cost when computing the plan’s COBRA premium. The IRS has indicated the fee is, however, a tax-deductible business expense for employers with self-funded plans.
The filing and remittance process to the IRS is straightforward and is largely unchanged from last year. On page two of Form 720, under Part II, the employer needs to designate the average number of covered lives under its “applicable self-insured plan.” The number of covered lives is multiplied by $2.17 (for plan years ending on or after Oct. 1, 2015) to determine the total fee owed to the IRS.
The Payment Voucher (720-V) should indicate the tax period for the fee is “2nd Quarter.” Failure to properly designate “2nd Quarter” on the voucher will result in the IRS’s software generating a tardy filing notice, with all the incumbent aggravation on the employer to correct the matter with IRS.