Page 1 of 1
The Affordable Care Act (ACA) established Health Insurance Marketplaces (also called Exchanges) where individuals can shop and enroll in health coverage. Individuals who meet certain criteria are eligible for premium subsidies and cost-sharing reductions for coverage on the Marketplace.
For the first time, in 2016 some employers will receive a notice from a Marketplace indicating that one of their employees signed up for health coverage through the Marketplace and received advanced premium subsidies. Many employers are asking what these notices mean and what actions they should take if they receive one.
Premium subsidies and cost-sharing reductions are designed to expand healthcare coverage by making insurance, and its utilization, more affordable. Premium subsidies, more accurately referred to as a premium tax credit, are claimed on an individual’s income tax return at the end of the year. What is unique about this tax credit is that an individual can choose to have the expected premium tax credit advanced throughout the year, in which case the government makes payments directly to the health insurer on the individual’s behalf. Importantly, individuals who have access to health coverage through an employer that is affordable and meets minimum value are not eligible to receive the premium tax credit or advances of the premium tax credit for their coverage.
The ACA generally requires that applicable large employers – generally employers with 50 or more full-time employees, including full-time equivalents – offer health coverage that is affordable and of minimum value to their full-time employees (and their dependents) or face an Internal Revenue Service (IRS) tax. This is often referred to as the employer “pay or play” or employer mandate provision. Tax liability under this employer provision is triggered if one of the employer’s full-time employees receives a premium tax credit and the amount of the tax liability is determined by the number of full-time employees who received the premium tax credit.
During the Marketplace application process, individuals are asked a host of questions, including questions about access to health coverage through an employer. If the Marketplace determines that the individual does not have access through an employer to coverage that is affordable and meets the required minimum value, and assuming the individual meets other eligibility criteria, advance payments of the premium tax credit can begin.
In such an instance, the Marketplace is required to send the employer a Marketplace notice. This will be the first year the Federally Facilitated Marketplace (FFM) is sending out these notices. It is worth noting that there is not a commitment to send a notice to all employers, and the FFM has said it can send a notice only if the individual provides a complete employer address. Consequently, some employers expecting Marketplace notices may not receive them and notices may not be mailed to the preferred employer address.
The Marketplace notices will give employers advance warning that they may have potential tax liability under the employer mandate of the ACA. However, there are reasons that receiving a notice does not necessarily mean the IRS will be in hot pursuit, including:
The FFM recently posted a sample of its 2016 notice which can be found here.
Please note that the notice suggests that employers should call the IRS for more information if they have questions, however, IRS telephone assistors will be unable to provide information on the Marketplace process, including the appeals process, and will be unable to tell an employer whether they owe a tax under the employer mandate.
An employer who receives a Marketplace notice may want to appeal the decision that the individual was not offered employer coverage that was affordable and of minimum value. An employer has 90 days from the date of the notice to file an appeal, which is made directly to the Marketplace. Importantly, the IRS will independently determine whether an employer has a tax liability, and the employer will have the opportunity to dispute any proposed liability with the IRS. Similarly, an individual will have the opportunity to challenge an IRS denial of premium tax credit eligibility. Any contact by the IRS, however, will occur late in the game after the year’s tax liabilities have already been incurred. Therefore, although an appeal is not required, it may be advisable.
Regardless of whether an employer pursues an appeal, an employer, particularly one that offers affordable, minimum value health coverage, should communicate to its employees about its offering. Although an applicable large employer is required to furnish IRS Form 1095-C to full-time employees detailing the employer’s offer, a better option is providing employees with information before they enroll in Marketplace coverage.
In summary, the Marketplace notice serves as an advance warning that either the employer or the employee may have a tax liability. Given this exposure, employers should review Marketplace notices and their internal records and consider taking action.
Beginning January 1, 2015, employers have new reporting obligations for health plan coverage, to allow the government to administer the “pay or play” penalties to be assessed against employers that do not offer compliant coverage to their full-time employees.
Even though the penalties only apply if there are 100 or more employees for 2015, employers with 50 or more full-time equivalent employees are required to report for 2015. Also, note this reporting is required even if the employer does not maintain any health plan.
Employers that provide self-funded group health coverage also have reporting obligations, to allow the government to administer the “individual mandate” which results in a tax on individuals who do not maintain health coverage.
These reporting obligations will be difficult for most employers to implement. Penalties for non-compliance are high, so employers need to begin now with developing a plan on how they will track and file the required information.
Pay or Play Reporting. Applicable large employers (ALEs) must report health coverage offered to employees for each month of 2015 in an annual information return due early in 2016. ALEs are employers with 50 or more full-time equivalent (FTE) employees. Employees who average 30 hours are counted as one, and those who average less than 30 hours are combined into an equivalent number of 30 hour employees to determine if there are 50 or more FTE employees. All employees of controlled group, or 80% commonly owned employers, are also combined to determine if the 50 FTE threshold is met.
Individual Mandate Reporting. Self-funded employers, including both ALEs and small employers that are not ALEs, must report each individual covered for each month of the calendar year. For fully-insured coverage, the insurance carrier must report individual month by month coverage. The individual mandate reporting is due early in 2016 for each month of 2015.
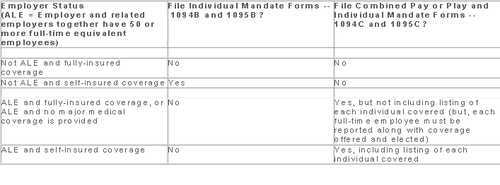
Which Form? ALE employers have one set of forms to report both the pay or play and the individual mandate information – Forms 1094C and 1095C. Insurers and self-insured employers that are not ALEs use Forms 1094B and 1095B to report the individual mandate information. Information about employee and individual coverage provided on these forms must also be reported by the employer to its employees as well as to COBRA and retiree participants. Forms 1095B and 1095C can be used to provide this information, or employers can provide the information in a different format.
The following chart summaries which returns are filed by employers:
Who Reports? While ALE status is determined on a controlled group basis, each ALE must file separate reports. Employers will need to provide insurance carriers, and third party administrators who process claims for self-funded coverage (if they will assist the employer with reporting), accurate data on the employer for whom each covered employee works. If an employee works for more than one ALE in a controlled group, the employer for whom the highest number of hours is worked does the reporting for that employee.
Due Date for Filing. The due date of the forms matches the due dates of Forms W-2, and employers may provide the required employee statements along with the W-2. Employee reporting is due January 31st and reporting to the IRS is due each February 28th, although the date is extended until March 31st if the forms are filed electronically. If the employer files 250 or more returns, the returns must be filed electronically. Reporting to employees can only be made electronically if the employee has specifically consented to receiving these reports electronically.
Penalties. Failure to file penalties can total $200 per individual for whom information must be reported, subject to a maximum of $3 million per year. Penalties will not be assessed for employers who make a good faith effort to file correct returns for 2015.
What Information is Required? For the pay or play reporting, each ALE must file a Form 1094C reporting the number of its full-time employees (averaging 30 hours) and total employees for each calendar month, whether the ALE is in a “aggregated” (controlled) group, a listing of the name and EIN of the top 30 other entities in the controlled group (ranked by number of full-time employees), and any special transition rules being used for pay or play penalties. ALE’s must also file a 1095C for each employee who was a full-time employee during any calendar month of the year. The 1095C includes the employee’s name, address and SSN, and month by month reporting of whether coverage was offered to the employee, spouse and dependents, the lowest premium for employee only coverage, and identification of the safe-harbor used to determine affordability. This information is used to determine pay or play penalty taxes and to verify the individuals’ eligibility for subsidies toward coverage costs on the Federal and state exchanges.
If the ALE provides self-funded coverage, the ALE must also report on the 1095C the name and SSN of each individual provided coverage for each calendar month. If an employer is not an ALE, but is self-funded, the name and SSN of each covered individual is reported on the 1095B and the 1094B is used to transmit the forms 1095B to the IRS.
A chart is available that sets out what data must be reported on each form, to help employers determine what information they need to track. Click here to access the chart.
Next Steps. Employers will need to determine how much help their insurance carrier or TPA can provide with the reporting, and then the employer’s HR, payroll and IT functions will need to work together to be sure the necessary information is being tracked and can be produced for reporting in January 2016.
With Congress in its summer recess, now is a good time to reflect on the top ACA issues worth monitoring as 2015 quickly approaches. Here are a handful of key issues to watch:
Dueling Court Cases on Federal Subsidies
One issue grabbing national headlines is the dueling decisions coming out of the U.S. Court of Appeals for the District of Columbia (Halbig v. Burwell) and the U.S. Court of Appeals for the Fourth Circuit (King v. Burwell) on missing language in the ACA that would have authorized the federal government to provide premium subsidies to individuals who sign up for health plans through the federal Exchanges. The legal issue in these court cases is whether the ACA premium tax credit (aka subsidy) is available to those individuals who enroll in qualified health plans (QHP) through state operated Exchanges or if it is available only to those to enroll in a QHP through a federally funded Exchange.
A primary concern is that a significant number of people in about two-thirds of the states (who did not set up a state-run Exchange) rely on the subsidy to purchase a plan in the federal Exchange. Specifically, the ACA’s employer mandate penalty of $3000 is based upon an employer having an employee seek coverage through an Exchange and receive the federal premium subsidy. In general, the employer mandate requires that “applicable large employers” offer their full-time employees minimum essential coverage or potentially pay a tax penalty. However, according to the statutory text of the ACA, the penalties under the employer mandate are triggered only if an employee receives a subsidy to purchase coverage through an Exchange established by the states. Both cases are being appealed to higher courts and will likely be consolidated into one case to be heard by the U.S. Supreme Court in the not so distant future.
In an interesting development, a video surfaced last week featuring one of the ACA’s chief architects (John Gruber) saying that health insurance subsidies should only be available in those states who opt to build and implement state-based Exchanges to gain participation. The idea was to create an incentive to have states actively involved in the hosting of an Exchange, rather than relying on the federal government to operate the Exchanges in each state. Whether this video will be used as evidence to uphold the argument that subsidies can only be offered by state-based Exchanges remains to be seen.
Lack of Back End Software for Federal Exchange
Of course, one of the big news stories in 2013 and early 2014 was the substandard launch of the federal Exchange, which led to many Americans having to wait to be enrolled in an ACA-compliant health plan. Although some technical snafus have been addressed, there are many that still remain. For example, a top White House official recently told Congress that the automated system that is supposed to send premium payments to insurance companies is still under development, and they did not have a completion date for it yet. The lack of an electronic verification process is only one part of the “backend” software that is still problematic five years after PPACA was passed.
Future of Navigators in Comparison with the Value of Brokers
Several recent studies have touted the benefits of using third parties, such as Brokers, to help consumers find coverage under the ACA. Some of these studies have focused on the usefulness of using Brokers/Agents over the benefits of using Navigators. A recent Urban Institute study found that health insurance Brokers were the most helpful in providing health insurance Exchange information when compared to other types of resources, including Navigators and website content. However, there are other published studies showcasing how Navigators have been useful to consumers. That being said, Brokers have assumed an integral role supporting millions of Americans in securing and maintaining coverage for many decades, and continue to be knowledgeable resources, as they are licensed in the states they operate in, whereas Navigators are not required to meet the same licensing standards as Brokers/Agents. It will be interesting to see what the future holds for Navigators, who are not as experienced and who are, in the end, dependent upon federal grants to provide their services.
Provider Access Issues & Emergency Room Over-Usage
A number of public policymakers have raised concerns recently about the fact that there are shortages of key physicians and other providers and as a result is causing a increase in non-emergent patient visits to expensive ER departments. A recent story in the New York Times highlighted similar concerns, saying the ACA cannot change the fact that visiting an emergency room may be easier than seeing a primary care physician in some instances or locations. Other stories and studies highlight how the ACA and health care reform initiatives can affect access to providers in many different ways, such as changing reimbursement levels, improving the availability of certain types of specialists, or re-educating the patient to move from visiting the ER department to either making an appointment ahead-of-time or visiting a less expensive Urgent Care center for care.
Premium Rate Increases
Another critical issue to monitor are premium increases that might be occurring in spite of the initial promises that the ACA would lower health care costs. Health plans have begun publishing proposed rates for 2015, resulting in a recent flurry of news articles and reports addressing the impact of the ACA on insurance premiums.
The Wall Street Journal published a front page report discussing the ACA’s impact on premium increases earlier this summer, saying, “Hundreds of thousands of consumers nationwide, who bought insurance plans under the Affordable Care Act, will face a choice this fall: swallow higher premiums to stay in their plans or save money by switching.”
The Journal goes on to say that a new picture is emerging in 10 states where 2015 premium insurance rates for individual plans have been filed, “In all but one (state), the largest health insurer is proposing to increase premiums between 8.5% to 22.8% next year.” Ironically, smaller health plans are reducing their 2015 rates in the same market in an attempt to gain market share.
The significance of this trend is underscored in a statement released earlier this summer by Karen Ignagni, president & CEO of America’s Health Insurance Plans (AHIP), in which she expressed concerns about keeping health insurance affordable for patients. “Affordability remains a top priority for consumers when it comes to their health care,” she said.
Bonus: Be Sure To Watch The Political Races
With the ACA’s continued challenges, the ups and downs of the U.S. economy, key world events in the Middle East, and other confounding variables, one has to wonder what will happen during the mid-year elections this fall. As reported by CNN and other news outlets, the ACA became an key issue in Obama’s 2012 re-election victory as well as Democrats picking up seats in the Senate and House in that election.
As November 3, 2015 approaches, many different messages could be sent back to the White House and Congress. If Republicans take over the Senate and retain control of the House, how will this impact the ACA over the next several years? If the congressional houses remain split, we may have less going on by either political party. How will the state-level elections impact the ACA and state-run Exchanges? Only time will tell.